Adolescent Medicine
The Division of Adolescent Medicine at SickKids is dedicated to improving adolescent health. Our mission is to provide the best in inclusive, compassionate and developmentally sensitive care, to advance the understanding of the specific health needs of youth in Canada and to prepare the next generation of leaders in adolescent health.
The interprofessional Adolescent Medicine team provides comprehensive care for youth with eating disorders, pregnant and parenting teens, transgender youth, and substance use. Consultation is available for youth with a range of adolescent health concerns, particularly in the context of chronic health conditions. The division maintains active clinical care in inpatient, day treatment and outpatient settings.
Our vision is to be a world leader in the field of adolescent health by providing exemplary care, and contributing to the development of new knowledge through advocacy, training, education and research. Adolescent medicine team members are actively engaged in quality improvement, teaching and research initiatives.
What we do
The Division of Adolescent Medicine is committed to providing high quality, developmentally-appropriate clinical care to youth and their families through our specialty clinical programs. See our model of care at a glance (pdf) and information on our general consultation services, specialized assessment and treatment programs, and eating disorder units.
- Adolescent Medicine Consultation Clinic
- Complex Contraception Clinic
- Chronic health conditions
The team partners in many clinics across the organization including Lupus, STOMP (weight management), Sickle Cell, Sleep Disorders, Oncology, Kidney Transplant, and Heart Transplant clinics.
- Substance Use Program
- The Young Families Program
- Gender Care Clinic (with Endocrinology)
- Eating Disorders In-patient Unit
- Eating Disorders Day Hospital
- Eating Disorders Clinic
- STOMP Clinic
Programs and services
Expand the sections below to learn more about each of our programs and services in Adolescent Medicine, including applicable referral processes and additional resources.
The Eating Disorders Program at SickKids diagnoses and treats children and adolescents with a range of eating disorders. We are the primary treatment site for the central Toronto area and are a specialty centre for the province of Ontario. Our program has an interdisciplinary approach to treatment, meaning care is provided by a wide variety of health care specialists. We believe family involvement is crucial for eating disorder recover.
Who we see
- Ages 8 to 18 (new referrals accepted up to 17 years, 3 months).
- Males and Females.
- Those struggling to eat enough to stay healthy, with concerns about their body weight or shape, or with unhealthy behaviors related to weight control.
- We do not see young people with lifelong stable picky eating or pica/rumination issues exclusively. We do not treat young people with obesity due to binge eating.
Referral
- All patients require a referral to visit our clinic.
- If you are a health-care professional, log in to eCHN to submit your referral. From your eCHN account, you will be seamlessly connected to SickKids e-referral platform, EpicCare Link. Learn more about our referral process, including urgent referrals.
Our assessment process
The goal of the eating disorder assessment is to determine 1) Does the child or adolescent have an eating disorder? 2) If there is an eating disorder present, how medically ill is the child or adolescent? 3) If there is an eating disorder, what type of treatment do we recommend?
It is optimal that the assessment be attended by all custodial parents/guardians. Many care providers are involved in the assessment, including a nurse, psychologist, dietitian and medical provider (MD or NP). Learners in any of these fields may also be involved.
Following the assessment, we will offer the best treatment option – either offered through our program or other interventions.
What we offer
Eating Disorders Inpatient Program
The Inpatient Unit is primarily designed to medically stabilize young people with serious eating disorders. The focus of the inpatient stay is on restoring health to the point that treatment can begin in the outpatient setting. Treatment includes medical monitoring, nutritional rehabilitation, psychiatric consultation and group programming.
Eating Disorders Outpatient Program
Outpatient treatment of young people with eating disorders usually involves family therapy with a specialized therapist, along with medical monitoring by an adolescent medicine provider. Consultation with a dietitian and a psychiatrist is also available to those participating in the program.
For children less than 13 years of age, we offer the Children’s Outpatient Program for Eating Disorders (COPE Clinic) which offers care focused on the unique needs of the youngest eating disorder patients. Treatment is similar to that offered in the Outpatient Program, but also includes a multifamily group and separate groups for the parents and their child.
Eating Disorders Day Hospital (EDDH)
The EDDH provides specialized care for young people with severe eating disorders who have already received treatment in a ministry funded eating disorders program and need longer term intensive support for recovery. The EDDH program operates five days per week and the average length of treatment is six months. Regular family involvement is required. Referral to the EDDH must come from an eating disorders care provider who has been treating the young person involved.
Family education
For families participating in our treatment programs, we offer a two-part family education series. Part one teaches what an eating disorders is, the possible medical complications, the approach to nutritional recovery and describes the treatment we offer. Part two focuses on how parents/guardians can support their child with an eating disorder to resume normal eating (meal support). Families will receive information about family education at their assessment or initial meetings with their care providers.
Education
We provide education to future care providers through their specific discipline (medicine, nursing, psychology, social work and dietetics). Please contact your specialty’s hospital department for more information.
Research
As part of an academic centre, we are often pursuing research projects. Families may be approached about participation in research aimed at improving our knowledge and treatment of paediatric eating disorders. Participation in research is not required to be part of our program and refusal to be part of a study will not affect treatment.
The Substance Use Program provides Day Treatment Services and Outpatient Services.
Through both services, the program provides:
- Assessment and treatment for teens up to 18 years of age.
- A parent program and support for families or guardians of teens in the program - upcoming parent group dates will be announced soon.
- Comprehensive health assessment and medical follow-up as needed.
- Education about adolescent alcohol and substance use and substance use disorders.
Substance Use Outpatient Services
- Outpatient counselors provide assessments and short and long-term individual and/or parent counselling.
- Outpatient staff are also available to facilitate education sessions around issues relating to substance use and use for community organizations or teams.
- Health assessment and education, with ongoing follow-up available from paediatricians.
Substance Use Day-Treatment
- The program hours are Monday to Friday during the school year from 9 a.m. to 3 p.m.
- There is a maximum of 8 to 10 teens in the program.
Individual treatment is aimed at reducing or eliminating substance use in accordance with the program’s harm reduction philosophy. - An academic program is available with opportunities for the teens to work towards secondary school credits with the Toronto District Secondary School teacher, instructing Ministry of Education curriculum.
- Daily treatment groups, life skills instruction and ongoing individual counselling and support are also available.
- Health assessment and education, with ongoing follow-up available from paediatricians. Programming that promotes involvement with healthy non-substance related activities.
Substance Use Day-Treatment Summer School Program
The Substance Use Day Treatment Program is a unique opportunity for teens who recognize their alcohol and/or substance use has impacted their lives and are looking to make changes. Our summer program offers a blend of therapeutic, individual and group support while simultaneously working on attaining an academic credit.
Our program offers:
- Day Treatment for teens who are looking to make changes in regards to their substance use using a Harm Reduction Model
- Are interested in attaining a Secondary School Credit with a Toronto District Secondary School teacher
- Have an adult to support them while in the program
- Access to health care and individual counselling
- Possible placement for full time program in September
For more information about the Day Treatment Summer Program please call (416) 813 5097 or (416) 813 8854.
Substance Use Parent Support
Parent education and support is a core aspect of our programming. Parents are often at a point where they are no longer sure what they should or should not be doing to help their teen. They may be exhausted, managing other family and life stresses, and extremely worried about their teen.
Virtual Caregiver Group:
This is a group for family members who are supporting a youth who is struggling with difficulties relating to substance use. The program offers education, support and skills development.
Family members will learn about, discuss and practice skills such as coping, grieving, dealing with emotions, solving problems, setting goals, communicating and setting limits.
Goals include:
- To build an understanding of various factors related to adolescent substance use.
- To learn concrete strategies to best support teens who use substances.
- To prevent your own burnout and engage in self-care while supporting your teen.
Next group dates: TBA
CareConsult for Youth Substance
Launched this January 2026, CareConsult for Youth Substance is a program that provides professional-to-professional virtual consultation services for health care professionals (HCPs) working with youth up to 25 years of age who have substance use health needs or substance use disorders located in the Greater Toronto Area (GTA).
Learn more about CareConsult for Youtube Substance See other available resources
Advocacy
Members of our program are involved with local, provincial and national initiatives that involve advocacy for young people and their families who are experiencing difficulties relating to alcohol and other substance use.
Research
- Long-term outcomes of SickKids’ Substance Use Day Treatment Program.
- Examining the use of a short screening questionnaire to better understand the issues relating to mental health and substance use for patients in the Substance Use program.
- Strengthening families for parents and youth 12 to 16 years of age (a Health Canada Drug Strategy – community initiatives).
- Screening adolescents with chronic conditions for concurrent mental health and substance use difficulties.
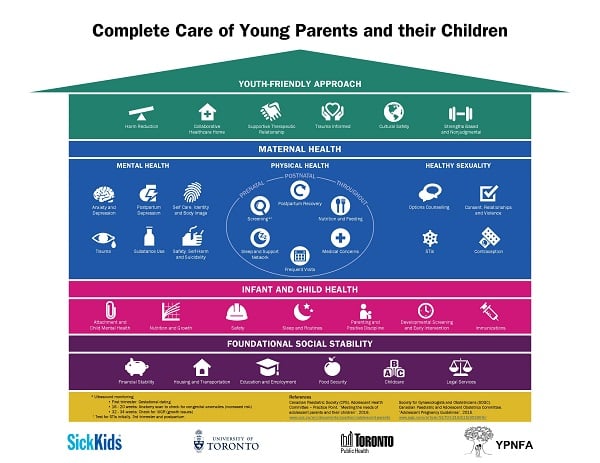
The Young Families Program is a health-care service for adolescent mothers and their children. Our program acts as the medical home for both the mother and infant and will follow the family until the child/children reaches two to three years of age. The services provided include comprehensive health care, management of acute/chronic illness, nutrition or feeding concerns, parenting education and support, sexual health, psychosocial/mental health support, and co-ordination of care with community partners.
Our team consists of paediatricians, a nurse practitioner, registered nurse, public health nurse, social workers and a psychiatrist.
Adolescents may be referred at any stage of pregnancy or after delivery by other health-care providers, community agencies or by the adolescents themselves. Referral guidelines include parenting women under 19 years of age who would benefit from support with parenting, complex medical needs, sexual health, and psychosocial concerns including mental health.
This program is affiliated with the Young Parents Program in the Gynecology Clinic, a prenatal program providing prenatal care to adolescents. The Young Families Program and Young Parents Program work closely along the continuum from pregnancy to parenting. For more information, please call 416-813-7779.
The infographic below outlines the unique health-care needs of adolescent-led families. It is a tool for clinicians interested in better understanding and empathizing with patients, as well as pregnant and parenting teens who may not feel comfortable communicating these needs. This resource was a joint effort between SickKids, Young Parents No Fixed Address (YPNFA), Toronto Public Health, and the University of Toronto.
Resources
View our Prezi presentation: How to use the Complete Care of Young Patients and their Children infographic
The Adolescent Medicine Consult Clinic (AMCC) provides youth with access to expert adolescent health-care services from our team of highly skilled interprofessional health-care providers. The team addresses a wide spectrum of concerns including illness-specific issues for youth with chronic health conditions, the identification and reduction of high-risk health behaviours and advocacy efforts.
Increasingly, the AMCC team is being consulted regarding youth with clinical conditions that are considered diagnostic dilemmas. In addition, AMCC continues to offer health care for marginalized and at-risk populations: lesbian, gay, bisexual, and transgender (LGBT2SQ+) youth, street-involved teens, and immigrant and new-comer adolescents to Canada.
AMCC also provides clinical services in collaboration with renal, cardiac and lung transplant programs, the HIV, SLE and Healthy Living clinics and through in-patient consultations. AMCC works with the Substance Abuse Program to address the often complex health needs of the adolescents in the program.
AMCC continues to build partnerships with local agencies such as Toronto Children’s Aid Society, St. Stephen’s Community House and the Triangle School Program of the Toronto District School Board in an effort to enable youth-at-risk in the downtown core to access health information and necessary health services otherwise unavailable to them. AMCC health care professionals continue to provide outreach and community education to various agencies such as York Family Services and schools in the Toronto District School Board.
The Continuity Clinic for fellows in Adolescent Medicine subspecialty continues to focus on continuity of care for medical services, ongoing counselling to youth and enhancing the ability for successful interventions.
Learn more about the Gender Care Clinic and access related resources.
Learn more about the Sexual health Promotion and Resource (SPaRC) Clinic and access related resources.
Key staff
Division Head:
Subspecialty Residency Training Program Director:
Vandana Rawal
Subspecialty Residency Training Associate Program Director:
Karen Leslie
- Marian Coret
- Eudice Goldberg
- Debra Katzman
- Sarah Kearny
- Chana Korenblum
- Karen Leslie
- Vandana Rawal
- Cathleen Steinegger
- Jessica Teicher
- Alene Toulany
- Trisha Tulloch
- Ashley Vandermorris

Research activities are integral to members within the Division of Adolescent Medicine.
The types of projects that are currently being conducted include understanding early-onset eating disorders, medical complications of eating disorders, clinical outcomes for adolescents with anorexia nervosa and bulimia nervosa, interventions aimed at the health and developmental needs of high-risk children of teen parents, faculty mentorship, effective approaches to treating adolescents with heroin/opiate addiction, outcome in a substance use day treatment program, health values and chronic illness, effectiveness of HIV prevention education with incarcerated youth, information technology for health promotion with youth and Web-based treatment resources for HIV-positive youth.

Our division provides clinical teaching for medical students, residents, fellows, and other interdisciplinary trainees.
Teaching includes weekly sessions on substance use, twice weekly teaching sessions on a broad variety of adolescent medicine topics, weekly divisional rounds, weekly discussions led by the fellows and weekly meetings with the clinic social worker.
Continuing medical education and public education are also priorities for the division. SickKids plays an important role in the training of students in nursing, medicine, social work, psychiatry addition to the trained professionals who will be supervising them.
The section below details educational and training offerings from Adolescent Medicine including description, application process and eligibility requirements.
The Division of Adolescent Medicine at The Hospital for Sick Children and University of Toronto offers a Royal College of Physicians and Surgeons of Canada (RCPSC) accredited subspecialty training program in Adolescent Medicine.
This two-year program prepares individuals for an academic career in Adolescent Medicine. The program facilitates the development of clinical, educational, research and administrative skills, as well as supports the development of leadership expertise in the field. The Division also offers clinical fellowship training (for periods of up to two years) for individuals from countries outside of North America who are interested in obtaining additional training in Adolescent Medicine in order to inform their work in this field in their home country.
The first year of the training program is designed to foster the development of a theoretical foundation and core skills in Adolescent Medicine that is supported by clinical experience. The clinical responsibilities include outpatient experiences (hospital and a variety of community-based settings), inpatient experiences, and consultation on outpatients and hospitalized patients in medical, surgical and psychiatric settings. These clinical experiences provide the trainee with exposure to a breadth of complex clinical issues including adolescent sexual health, eating disorders, substance abuse, teen pregnancy and parenting, complex medical and psychosocial problems, and chronic illness and disability. First year subspecialty trainees will also develop a repertoire of research skills through the critical analysis of current literature in the field, and development of a research project. The trainee is expected to define his/her area of research with supervision from a designated faculty member, then pursue this area of interest during the latter part of the first year. The first-year trainee also has the opportunity to develop his/her teaching skills, and is expected to participate in the formal teaching program of the Division.
The second year of sub-specialty training is meant to refine the clinical, educational, administrative and research skills acquired over the previous year in preparation for transition to practice. The trainee has an enhanced role in the teaching program of the Division and is given the opportunity to precept and supervise residents and medical students in both the outpatient and inpatient settings. During the second year, the trainee is also expected to continue and complete the clinical research project that began in their first year. Additionally, the trainee spends time focusing on developing leadership skills in the area of Adolescent Medicine.
Application process
CaRMS eligible applicants:
Applicants to Adolescent Medicine who are eligible for RCPSC recognition of their paediatric and subsequent subspecialty training must apply through the subspecialty resident CaRMS match. The details of this process are described on the Canadian Residency Matching Service. Applicants will not be considered for subspecialty training without going through the CaRMS match.
International applicants:
Applicants who do not meet eligibility criteria for RCPSC recognition can apply to the Division of Adolescent Medicine for a clinical fellowship position if they have successfully completed a minimum of three years of paediatric training. Applicants should be aware that funding for these clinical fellowship positions is extremely competitive. All candidates with training from outside North America are strongly encouraged to undertake an elective with the Division of Adolescent Medicine.
Only those candidates who have submitted all required documentation including their curriculum vitae, application form, references and have been offered an interview will be considered for a position. Applications are completed online.
Apply online Fellowship Application - Adolescent Medicine
For more information, please email: adolmed.trainingprogram@sickkids.ca
Dr. Vandana Rawal
Program Director, Division of Adolescent Medicine
Email: Vandana.Rawal@sickkids.ca
Dr. Karen Leslie
Associate Program Director, Division of Adolescent Medicine
Email: Karen.Leslie@sickkids.ca
Or
Akta Sehgal
Education Coordinator, Division of Adolescent Medicine
Tel: 416-813-7654 ext. 414567
Fax: 416-813-5392
Email: adolmed.trainingprogram@sickkids.ca

