Marrow Failure and Myelodysplasia (Pre-leukemia) Program
The Marrow Failure and Myelodysplasia (Pre-leukemia) Program (MFMP) aims to provide state-of-the art care for patients with bone marrow failure and myelodysplasia syndromes (MDS or pre-leukemia) and promote leading-edge research and education. Established in 2001, it is the first of its kind in Canada.
The MFMP is a multi-disciplinary program designed to apply the emerging science of blood cell formation and genetics to patient care. It provides unique opportunities for laboratory and clinical research and education of trainees from around the world to enhance their expertise.
Who we are
MFMP collaborates with multiple clinicians and scientists in Canada and abroad to expedite research and to advance knowledge in the field.
- Conrad Fernandez
- Catherine Corriveau-Bourque
- Geoff Cuvelier
- Roona Sinha
- Robert Klaassen
- Lisa Goodyear
- Meera Rayar
- Josee Brossard
- Vicky Breakey
- Bruno Michon
- Mariana Silva
- Soumitra Tole
- Yves Pastore
- Sharon Abish
- MacGregor Steele
- Jeffrey Lipton
- Michaela Cada
- Jodie Odame
- Rinu Mathew
- Sarah Ogle
- Briar O’Neil
- Susan Macphee
- Lilian Luik
- Hongbing Li
- Christian Youn
Referral guidelines
MFMP accepts referrals of patients with acquired or inherited bone marrow failure or myelodysplastic syndromes from the Greater Toronto Area as well as requests for consultation (second opinion) from other sites.
What we do
Objectives
- Meet the clinical needs of patients and families with acquired and inherited bone marrow failure and myelodysplastic (pre-leukemia) syndromes.
- Advance laboratory and clinical research so that novel developments in understanding the biology of the diseases are translated into clinical practice.
- Educate new physicians, researchers and other health care providers.
Our activities
MFMP includes a clinical service that provides diagnostic procedures, cancer surveillance, treatment, genetic counseling, nursing support, social support and nutritional counseling. Research studies are designed to address clinical and biological questions in the field.
Clinical care
- Develop standard-of-care guidelines for the clinical management of patients, including diagnostic procedures, treatments and surveillance for complications
- Counsel patients and families who are referred from other centers across Canada or abroad
Research
- Identify and study the functional characteristics of genes and proteins associated with inherited bone marrow failure syndromes, myelodysplasia and leukemia
- Study the clinical characteristics, disease course and treatments of the disorders
Education
- Train the new generation of researchers, physicians and other health-care providers in the field of bone marrow failure and myelodysplasia
- Coordinate educational initiatives for patients and families including the annual Marrow Failure and Myelodysplasia Patient and Family Conference
The program acts as a training resource for students and postdoctoral clinical and basic research fellows. It provides an excellent infrastructure for lab-based and clinical research in marrow failure syndromes and MDS, through its research laboratories, clinic, its national collaborative network, the Canadian Inherited Marrow Failure Registry, and its international collaboration through the Severe Congenital Neutropenia Advisory Board.
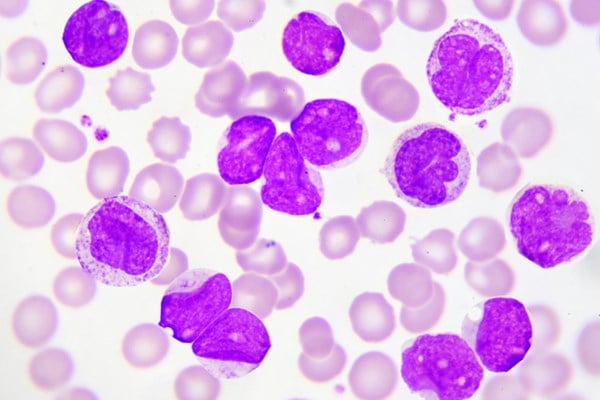
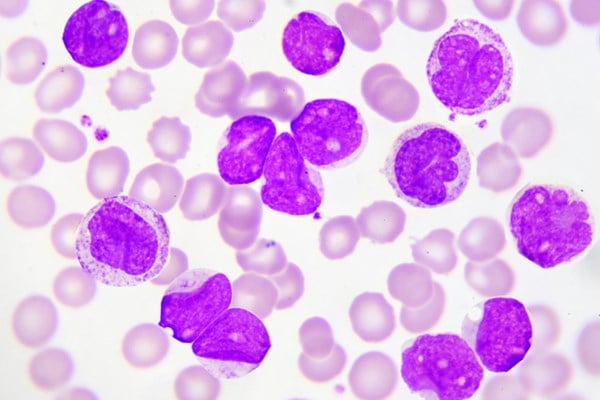
Classification of marrow failure and myelodysplasia syndromes
- Fanconi anemia, Shwachman-Diamond syndrome, dyskeratosis congenita, congenital amegakaryocytic thrombocytopenia, congenital hair hypoplasia, Pearson disease, reticular dysgenesis
- Diamond Blackfan anemia, sideroblastic anemia, congenital dyserythropoietic anemia
- Kostmann neutropenia, cyclic neutropenia, glycogen storage disease type Ib, Barth syndrome, myelokathexis
- Thrombocytopenia with absent radii syndrome, dyserythropoietic anemia with thrombocytopenia, familial thrombocytopenia with propensity for leukemia, other familial thrombocytopenias (e.g. non-syndromic familial thrombocytopenia)
- Acquired aplastic anemia
- Acquired single lineage cytopenia
- Acquired
- Inherited
Therapies offered by MFMP
Children and adults with bone marrow failure and MDS have low blood counts and are at high risk of developing leukemia. Therapies offered by the MFMP include:
- Platelet and blood transfusion
- Growth factors such as G-CSF or eltrombopag
- Corticosteroids such as prednisone
- Androgens such as oxymethalone
- Immunosuppressive therapy (ATG and cyclosporin)
- Chemotherapy such as azacitidine and hydroxyurea
- Haematopoietic stem cell transplantation from related or unrelated donors. Sources are bone marrow, peripheral blood or cord blood. This treatment is given in our highly-qualified and highly experienced blood and marrow transplantation unit.
Transitioning to adult care
The MFMP has built a clinical and research collaborative program with physicians at Princess Margaret Hospital and Sunnybrook Hospital. Patients with bone marrow failure or myelodysplasia who reach the age of 18 years as well as patients who are diagnosed with bone marrow failure in adulthood are treated at these facilities.
In addition to collaboration with clinics at Princess Margaret Hospital and Sunnybrook Hospital, we work with patients and their families to find appropriate adult haematology follow-up closer to home to make sure patients get the care they need, where they need it.
Research activities
Substantial advances have been made in identifying genes which are mutated in inherited marrow failure syndromes. However, our experience in the clinic is that many of the patients with these syndromes cannot be accurately classified as known syndromes. The prevalence of the unclassifiable syndromes, their clinical characteristics and the relationship to genes mutated in already categorized syndromes have never been studied.
We analyzed data from the Canadian Inherited Marrow Failure Registry to answer these questions and found that the unclassifiable syndromes constitute a major portion of the group of inherited marrow failure syndromes (about a quarter), and present major diagnostic and therapeutic dilemmas. We have also shown that patients with a previously unclassifiable marrow failure syndrome with defect in body balance and blood counts may have a disease called dyskeratosis congenita.
Leukemia and pre-leukemia (myelodysplastic syndromes, MDS) are common in marrow failure syndromes and have extremely poor outcomes, but the mechanism of leukemogenesis is unknown. We used Shwachman-Diamond syndrome (SDS) marrow cells as a model to study gene expression pattern which might be associated or possibly mechanistically related to leukemia. We have found that SDS marrow cells exhibit abnormal expression pattern of leukemia-related genes, which might result in continuous stimulation favoring evolution or progression of malignant cells.
We discovered that marrow stem cells are reduced in number, grow poorly, die prematurely and are hypersensitive to the cell death protein, Fas. We also showed that the SDS microenvironment is unable to support growth of normal marrow cells and is characterized by increased angiogenesis.
Certain patients with this pre-leukemic syndrome do not respond to treatment with Granulocyte colony stimulating factor (G-CSF). We have found that a novel mutation in the extracellular part of the G-CSF receptor molecule can lead to defective activation of the G-CSF pathway. Using cellular methods we showed that the abnormality can be corrected by prednisone and a successful regimen using a combination of G-CSF and prednisone was developed. Interestingly, we have found that such a mutation might offset of the pro-proliferative effect of pre-leukemic mutations in the intracellular domain of the receptor.
We showed that there has been a striking improvement in survival for paediatric patients treated with multi-agent immunosuppression in the last decade. However, transplantation results have also improved and this remains the first-line therapy for children with severe acquired aplastic anemia who do not have a matched relative donor for bone marrow transplantation. In addition, the risk factors for development of severe aplastic anemia are largely unknown. As a collaborative study with the USA National Institute of Health in Bethesda, the group showed that heterozygosity for SBDS mutations predisposes to severe aplastic anemia by accelerating telomere shortening via a telomerase-independent mechanism.
The accelerated apoptosis in inherited marrow failure syndromes inspired us to develop innovative, reduced-toxicity bone marrow transplantation regimens without radiation with promising preliminary results.
Through a collaborative work, a mouse model to study neutrophil engraftment after bone marrow transplantation was generated in Dr. Michael Glogauer’s laboratory at the University of Toronto.
Canadian Inherited Marrow Failure Registry (CIMFR)
The CIMFR is a national registry that collects blood, marrow samples and information to advance the understanding of inherited bone marrow failure syndromes.
The database has been the foundation for multiple publications tackling important medical problems, diagnostic dilemmas, and treatment of children with these conditions.
Publications
- Steele JM, Sung L, Klaassen R, Fernandez CV, Yanofsky R, Wu J, Odame I, Silva M., Champagne J, Ali, K, Brossard J, Samson Y, Abish S, Le D, Jardine L, Hand JP, Lipton JH, Charpentier K, Stephens D, Freedman M, Dror Y. Disease Progression in Recently Diagnosed Patients with Inherited Marrow Failure Syndromes: A Canadian Inherited Marrow Failure Registry (CIMFR) Report. Pediatr Blood Cancer 2006: 47(7): pp 918-925
- Teo JT, Klaassen R, Fernandez CV, Yanofsky R, Wu J, Champagne J, Silva M, Lipton JH, Brossard J, Samson Y, Abish S, Steele M, Ali K, Dower N, Uma Athale, Jardine L, Hand JP, Tsangaris E, Odame I, Beyene B, Dror Y. Clinical and genetic analysis of unclassifiable inherited bone marrow failure syndromes. Pediatrics 2008: 122(1): pp 139-148.
- Hashmi SK, Allen C, Klaassen R, Fernandez CV, Yanofsky R, Shereck E, Champagne J, Silva M, Lipton JH, Brossard J, Samson Y, Abish S, Steele M, Ali K, Dower N, Athale U, Jardine L, Hand JP, Beyene J, Dror Y. Comparative analysis of Shwachman-Diamond Syndrome to other Inherited Marrow Failure Syndromes. Clin Genet. 2011: 79(5): pp 448-58
- Tsangaris E, Klaassen R, Fernandez CV, Yanofsky R, Shereck E, Champagne J, Silva M, Lipton JH, Brossard J, Samson Y, Abish S, Steele M, Ali K, Dower N, Athale U, Jardine L, Hand JP, Stephen D, Odame I, Canning P, Allen C, Carcao M, Beyene J, Roifman CM, Dror Y. Genetic analysis of inherited bone marrow failure syndromes from one comprehensive and population-based cohort and identification of novel mutations. J Med Genet 2011: 48(9): pp 618-28
- Ghemlas I, Li H, Zlateska B, Klaassen R, Fernandez CV, Yanofsky RA, Wu J, Pastore Y, Silva M, Lipton JH, Brossard J, Michon B, Abish S, Steele M, Sinha R, Belletrutti M, Breakey VR, Jardine L, Goodyear L, Sung L, Dhanraj S, Reble E, Wagner A, Beyene J, Ray P, Meyn S, Cada M, Dror Y. Improving diagnostic precision, care and syndrome definitions using comprehensive next-generation sequencing for the inherited bone marrow failure syndromes. J Med Genet 2015 Sept: 52(9):575-84
- Waespe N, Dhanraj S, Wahala M, Tsangaris E, Enbar T, Zlateska B, Li H, Klaassen RJ, Fernandez CV, Cuvelier GDE, Wu JK, Pastore YD, Silva S,. Lipton JH, Brossard J, Michon B, Abish S, Steele M, Sinha R, Belletrutti MJ, Breakey VR, Jardine L, Goodyear L, Kofler L, Cada M, Sung L, Shago M, Scherer SW, Dror Y. The clinical impact of copy number variants in inherited bone marrow failure syndromes. npj Genomic Medicine 2017 May 10;2
- Lauhasurayotin S, Cuvelier GD, Klaassen RJ, Fernandez CV, Pastore YD, Abish S, Rayar M, Steele M, Jardine L, Breakey VR, Brossard J, Sinha R, Silva M, Goodyear L, Lipton JH, Michon B, Corriveau-Bourque C, Sung L, Shabanova I, Li H, Zlateska B, Dhanraj S, Cada M, Stephen SW, Dror Y. Reanalysing genomic data by normalized coverage values uncovers CNVs in bone marrow failure gene panels. NPJ Genom Med. 2019; 4: 30
- Heidemann S, Bursic B, Zandi S, Li H, Abelson S, Klaassen RJ, Abish S, Rayar M, Breakey VR, Dhanraj S, de Borja R, Shlien A, Dick JE, Dror Y. Cellular and molecular architecture of hematopoietic stem cells and progenitors in genetic models of bone marrow failure. JCI Insight. 2020 Feb 27;5(4)
Funding
Thank you to all patients and families in the Marrow Failure and Myelodysplasia Clinic for their participation in our clinical, education and research activities. We thank all donors, support groups and grant agencies who have generously been supporting our research, including:
- Gala of Hope Fund
- Fanconi Anemia Canada
- Shwachman-Diamond Canada
- Neutropenia Support Association Inc.
- C17 Research Network and Cancer Candlelighters Canada
- Shwachman-Diamond Syndrome Foundation
- Shwachman-Diamond Project Inc.
- Anemia Instituted of Research and Education
- SickKids Foundation
- Canadian Institutes of Health Research
Support MFMP
If you wish to contribute to the work and research carried out on Bone Marrow Failure and Myelodysplasia please do so through SickKids Foundation. Tax receipts will be issued for all contributions over $20.
Online
Donate to MFMP online by specifying Marrow Failure and Myelodysplasia (Pre-leukemia) Program in the Additional Comments box.
By mail
Donations can be made payable by cheque to the Marrow Failure & Myelodysplasia (Pre-leukemia) Program and sent to the following address:
SickKids Foundation
525 University Ave
Toronto, ON
M5G 2L3
By phone
Credit card donations can be made by calling 416-813-6166 or 1-800-651-5825. Please mention that you would like to designate the donated funds to the Marrow Failure & Myelodysplasia (Pre-leukemia) Program.
Contact us
Email: cimf.registry@sickkids.ca
Phone: 416-813-7654 ext. 1587
Fax: 416-813-5327

