Choosing Wisely at SickKids
It has been estimated that, in North America, 20-30% per cent of the tests and therapies currently requested and prescribed are likely unnecessary, add no value to care, and may even cause harm. That's why SickKids has participated in Choosing Wisely Canada, a campaign to help clinicians and patients engage in conversations about unnecessary tests and treatments, since 2016.
SickKids has produced a total of 19 recommendations that are specific to paediatric hospital patients. The recommendations developed are based on best-practices and evidence of overuse or potential harm to patients.
Choosing Wisely news

SickKids earns highest recognition from Choosing Wisely Canada
“Leadership Status” recognizes excellence in patient-centered care and stewardship

SickKids launches fourth phase of Choosing Wisely recommendations
Choosing Wisely recommendations address overuse of medically unnecessary tests and treatments received by patients at the hospital.

SickKids’ Choosing Wisely program is helping reduce unnecessary testing, treatments and imaging
Lessons learned at SickKids could be applied in other paediatric settings interested in taking a similar approach.

Research shows the implementation of a standardized approach to UTI diagnosis and follow-up reduced misdiagnosis and antibiotic use.

Research shows the implementation of a standardized approach to UTI diagnosis and follow-up reduced misdiagnosis and antibiotic use.

Choosing Wisely: Research shows low-risk injuries can safely forego abdominal CT imaging
With the typical rise in child and youth injuries from outdoor activities expected this summer, new research is helping to guide clinicians when CT imaging is needed most to help avoid unnecessary testing.

Research at SickKids shows the vast majority of paediatric ankle injuries are low risk and don’t require X-rays during emergency department visits.

SickKids is launching a third list of Choosing Wisely recommendations to address the potential overuse of tests and treatments received by patients at the hospital.

SickKids named a Level 3 Choosing Wisely Canada Hospital
SickKids has been recognized as a Level 3 Choosing Wisely Canada Hospital for building an organization-wide culture of reducing unnecessary tests and treatments.

Engaging families in shared decision making is essential to examine the benefits and limitations of each treatment option for patients with newly diagnosed, typical immune thrombocytopenia (ITP).
With an increased emphasis on ‘choosing wisely’ and reducing unnecessary medical tests across the medical field, SickKids paediatricians examined the benefits and limitations for a specific type of test and reviewed the scientific evidence as to when it is actually helpful in improving patient care.

Ontario paediatric emergency departments order fewer low-value imaging tests than US counterparts
Lower use of imaging tests in Ontario paediatric emergency departments was not associated with higher rates of poor outcomes, suggesting that use may be safely reduced in the United States, according to a new study by researchers at ICES and SickKids.

In some types of cancers, tumour markers will decrease with treatment and are helpful in predicting outcomes, which is why researchers at SickKids set out to discover if tumour markers could adequately detect cancer relapse independently of imaging tests.
Growth plate fractures in children’s ankle injuries are much rarer than previously thought
A new study led by SickKids found that lateral ankle injuries in children without X-ray evidence of a fracture are most often sprains that can be easily treated with a removable splint.

Organizations that have achieved this designation have demonstrated the strongest commitment and highest achievement in leading change to reduce overuse through organizational leadership, culture change, mentorship, and an assurance of sustainability.
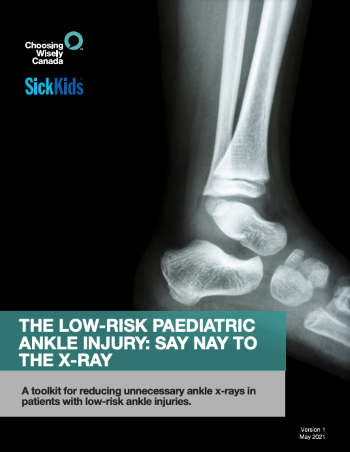
Say Nay to the X-ray
Choosing Wisely Canada mobilizes and supports clinicians and organizations committed to embedding campaign recommendations into practice. With their support, SickKids developed an evidence-based and easy to follow toolkit – “Say Nay to the X-ray” – which includes tools and methods to reduce unnecessary low-risk ankle imaging at paediatric emergency departments. The toolkit is available publicly to support quality improvement and decrease unnecessary tests and treatments in paediatric health care settings.
Download Toolkit (English) (PDF) Download Toolkit (French) (PDF)
Frequently asked questions for patients and families
As the Choosing Wisely movement in Canada had previously focused on adults without any formal recommendations for children (paediatrics), the goal of the Choosing Wisely initiative at SickKids is to encourage conversations about tests and treatments that may not be needed by creating recommendations that are specific to our young patient population and that resonate with paediatric care.
We will always continue to use appropriate tests for children who need them. The aim of Choosing Wisely is to reduce testing for children whose diagnosis and care will not be impacted by the results of tests. Many conditions can be identified by a simple examination. While tests can confirm a diagnosis, many do not impact the care that is provided due to the long wait time for results and other factors.
All the tests on Choosing Wisely lists are safe for patients. However, they simply may not be necessary for as many patients as they are currently being used for. The idea with Choosing Wisely is for health-care providers to think more carefully about how they will use the information from a test, if at all. If it's not going to be used, better to avoid the test.
Choosing Wisely Canada recommends four questions to ask your health-care provider:
- Do I [does my child] really need this test, treatment or procedure?
- What are the downsides?
- Are there simpler, safer options?
- What happens if I [we] do nothing?

