
Transplant and Regenerative Medicine Centre
Liver Transplant Program
The SickKids Liver Transplant Program is the largest paediatric liver transplant program in Canada and one of the busiest programs in North America. Our mission is to provide world-class comprehensive pre- and post-liver transplant care and superior clinical outcomes for infants, children and youth requiring liver transplant. Part of the SickKids Transplant and Regenerative Medicine Centre, the SickKids Liver Transplant Program is a leader in innovative paediatric liver transplant care, research, advocacy, and education.
The first liver transplant was performed at SickKids on October 12, 1986.
We perform anywhere from 25-40 transplants every year with over 700 transplants to date.
Outcomes surpass North American standards with a 97% survival rate 1 year post transplant and a 91% survival rate 10 years post-transplant.
Liver Transplant FAQ
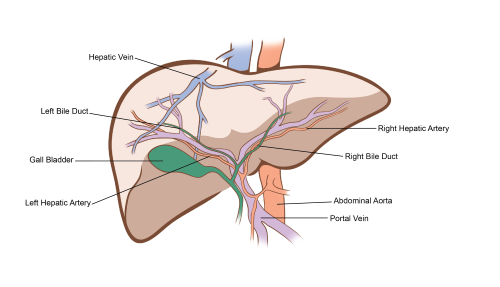
A liver transplant is an operation performed to replace a diseased or malfunctioning liver – in which all other medical interventions have been tried and failed – with a healthy piece of liver from another person. A donor liver may come for a deceased person who had previously decided (or whose family has decided) to donate their organs, or from a living person who is willing to donate a piece of their liver.
The liver transplant program at SickKids works closely with two organizations that facilitate liver donation in Ontario.
- Deceased Donation - The Trillium Gift of Life Network (part of Ontario Health) is responsible for coordinating organ and tissue donation and transplantation services.
- Living Donation – The Living Donor Liver Program run by University Health Network’s Ajmera Transplant Centre is responsible for the assessment and care of living donors. They have performed over 1,000 live donor operations and are world renowned for their living donor program.
There are many conditions that may lead to an infant, child or youth requiring a liver transplant. These include but are not limited to:
- End-stage liver disease resulting in life-threatening complications (ie. Biliary Atresia, Alagille Syndrome, PFIC)
- Metabolic conditions (ie. urea cycle defects, MSUD, PA, MMA)
- Inoperable tumours of the liver (ie. hepatoblastoma, hepatocellular caricoma)
- Acute liver failure
A referral needs to be made by your child’s primary care physician. This may be your child’s gastroenterologist, hepatologist, oncologist, metabolic physician, or surgeon. Please email liver.transplant@sickkids.ca for any additional information
Once a referral is received, one of our pre-transplant nurses will call you to discuss assessment for liver transplant. An assessment can be done as an outpatient over three to four days or as an inpatient based on the child’s needs. We strongly encourage all primary caregivers to attend the assessment, either in person or virtually.
During the assessment we will do tests to help the clinical team determine if:
- Your child needs a liver transplant
- There are any other treatment options that could prevent or delay transplant
- There are any other interventions that can improve your child’s outcomes following liver transplant
You and your child will meet a transplant physician, transplant surgeon, pre-transplant nurse, dietitian, physiotherapist, occupational therapist and social worker during the assessment process who will provide you with valuable information about liver transplant and how to care for your child both pre- and post-liver transplant.
We strongly recommend that all patients listed for liver transplant have received all the age-appropriate vaccines including COVID-19 vaccines (if eligible) prior to transplant. Immunization provides additional protection both before and after transplant when your child is more susceptible to infection. We often recommend additional vaccines or accelerated vaccination schedules prior to transplant to provide your child with as much protection as possible. Our clinical team would be happy to discuss your child’s immunization history and address any questions or concerns that you may have at the assessment.
Please bring your child’s immunization record to their liver transplant.
SickKids is privileged to work with the UHN Living Donor Liver Program.
Living donation offers the following benefits:
- Less time spent on the waiting list, which can reduce additional risks or complications that can develop the longer the patient is on the waiting list
- Lower chance of becoming sicker before transplant
- Potential for improved long-term outcomes
- Scheduled surgery time
Liver transplant surgery can take an average of 6-12 hours. Your child will be admitted to the Paediatric Intensive Care Unit (PICU) post-surgery and will be there for approximately 1-7 days. They will then be transferred to the multi-organ transplant unit where they will be admitted for 2-3 weeks. We will teach you about the post-transplant medications and how to care for your child when returning home and if required community resources.
The first 6 months to one year after liver transplant can be very busy. When you first leave the hospital, you can expect to return once to twice a week for follow up. We will slowly spread out visits depending on how your child is doing. For families who live far from the hospital, the clinical team will work with you to identify local resources to support your child; however frequent visits to SickKids will still be required.
On average by the time a child is one year post-liver transplant they will have bloodwork every 3 months and have clinic visits once to twice per year. The transplant team is always available to you should any issues or questions arise between visits. Once your child turns 18, they will graduate to an adult liver transplant program for ongoing follow-up care.
While deceased donation is confidential (i.e. the Deceased donor family will not know who their loved ones organs were directed to and you will not receive any identifying information about the donor), you may write a letter to the donor family if you choose. Some families and patients choose to write immediately after the transplant, some choose to write many years after transplant, and some choose not to do so. All are acceptable. Letters are to be anonymous and signed “from the recipient family” and no identifying information can be included. If you are interested, please ask the transplant nurses for further information and they will guide you on how to do so.

As a transplant program we would not be able to help so many children without our heroes – the generous donors and families that chose to donate their or their loved ones’ organs, including the selfless live donors who donate a piece of their liver to a child in need.
These donors are the reason our program is so successful and the reason so many children are thriving today. We thank you for your life-saving gift – on behalf of our clinical team, patients and their families!


UHN Living Donor Program
The Living Donor Program at University Health Network's Ajmera Transplant Centre care for people who would like to donate a kidney or a piece of their liver to a person with end stage kidney or liver disease.
Patient Referrals
For physician’s looking to refer patients to our program please complete the referral link. More information will be required once the link is completed; please ensure your contact information is correct.
Questions about referrals? Read here for more information to refer a patient to SickKids.
Meet the Liver Transplant Team
The Liver Transplant Team is a team of dedicated health-care professionals who want to help every child and family through the transplant process. Because SickKids is a teaching hospital, residents and fellows also care for patients.
In addition to their core care team, patients may also be supported by:
- Physiotherapists and occupational therapists
- Psychologists
- Dietitians
- Social workers
- Child life specialists
- and more!
Have questions for our team? Email us at liver.transplant@sickkids.ca
Physicians & Surgeons

Staff Physician, Medical Director, Paediatric Liver Transplantation

Staff Physician
Staff Physician

Mark Cattral
Transplant Surgeon
Anand Ghanekar
Transplant Surgeon

Staff Physician

Staff Physician
Mar Miserachs
Staff Physician

Transplant Surgeon
Allied Health & Nursing Team

Julia Celestini
Dietitian

Maria De Angelis
Nurse Practitioner

Julia Hensley
Social Worker

Alicia Nero
Patient Care Information Coordinator

Catherine Patterson
Physiotherapist

Alaine Rogers
Occupational Therapist

Stephanie So
Physiotherapist

Jennifer Stunguris
Pre-Transplant Nurse

Krista Van Roestel
Nurse Practitioner
Coming to SickKids
Prepare your child for their upcoming appointment or surgery by planning your visit to SickKids.




