A story of SickKids’ first scientist
Summary:
Perhaps there is no one who knows SickKids’ rich culture of collaboration better than one of its most longstanding scientists and the Hospital’s first basic scientist, Dr. Bibudhendra (Amu) Sarkar.
Crossing boundaries between science and medicine: the spirit of collaboration at SickKids
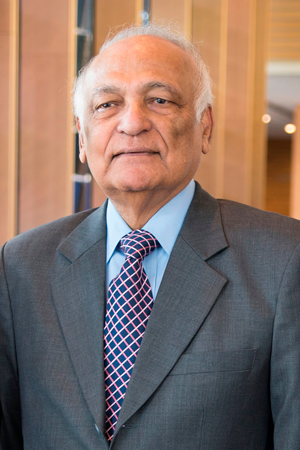
Perhaps there is no one who knows SickKids’ rich culture of collaboration better than one of its most longstanding scientists and the Hospital’s first basic scientist, Dr. Bibudhendra (Amu) Sarkar.
Sarkar joined The Hospital for Sick Children (SickKids) in 1964 at just 29 years old. SickKids’ Research Institute had officially formed in 1954, but it was clinical research that was predominantly being conducted by physicians as they sought innovative ways to improve diagnosis, treatment and care for children.
After meeting SickKids’ Dr. Andrew Sass-Kortsak at a conference in Chicago, Sarkar was invited to Toronto to give a scientific talk. As a basic scientist, he had no experience in medicine or paediatrics but his background in biophysics and inorganic biochemistry with a special interest in metal-protein interactions (which are biologically important molecules) was of great interest to Sass-Kortsak.
This was Sarkar’s first trip to Canada. Little did he know it would not only lead to a long career at SickKids, but also a new treatment for a rare genetic disease and come to represent the beginning of SickKids’ important history of collaboration between basic scientists and clinicians.
“As a young scientist, I was craving knowledge and was so interested in learning from my new colleagues. Andrew encouraged me to attend clinical rounds to learn more about the medical issues children faced. So while conducting my own research, I also went to rounds and learned as much as I could about medicine,” says Sarkar, who is now Senior Scientist Emeritus in Molecular Medicine at SickKids. “SickKids was a much smaller community in the early 60s. To the physicians, having a basic scientist around was such a novelty. I was curious and asked questions of almost everyone.”
Sass-Kortsak, who was a physician in clinical and metabolic genetics at SickKids, quickly became a mentor to Sarkar, meeting every morning before the day began. In line with Sarkar’s biochemistry background, Sass-Kortsak’s clinical interest was in the area of metal-caused diseases. For example, Wilson disease is a rare degenerative disorder that impacts how the body handles copper, which is vital for human survival, and results in copper deposits in the liver, brain and other tissues.

One day, he and Sarkar were discussing a patient with Wilson disease and Sass-Kortsak referred to some copper moving around freely within blood that is not bound to proteins. “I disagreed, I knew that copper has a high affinity for nitrogen, meaning it would need to look for another nitrogen compound to bind itself too. I thought this must not be different for copper in human blood? When I said this to Andrew, instead of pushing back, he simply said, ‘Okay, so show me.’ This was a seminal moment,” says Sarkar. “Andrew challenged me, so I started doing experiments with my own blood to prove my hypothesis.”
After much investigation, Sarkar’s hypothesis was right. He found that copper binds to an amino acid called histidine in human blood. This novel discovery, the isolation of copper-histidine in human blood, was published for the first time in Biochemistry of Copper published by Academic Press in 1966.
“This is how science progresses. Key questions at key moments that lead you to discovery,” says Sarkar. He continued working in this area and researching copper absorption in human cells, its interactions with proteins as well as uncovering its structure. The discovery led Sarkar to other diseases that are caused by abnormal copper absorption.
Menkes disease, another rare neurodegenerative disorder, is characterized by copper deficiency and results in early death. Children do not typically live longer than three years. “I started talking to Andrew about Menkes disease as it seemed to be the opposite of Wilson disease. While Wilson disease results in too much copper, kids with Menkes do not have enough,” says Sarkar.
In 1972, an Australian clinician discovered that Menkes was caused by copper deficiency. In 1976, Sass-Korstak diagnosed SickKids’ first patient, a premature infant, with Menkes disease. Because of their ongoing conversations about Wilson and Menkes diseases, Sass-Korstak immediately called Sarkar to discuss the case.
“While I was not a clinician, Andrew thought my research background could hold an important key for this patient. The baby was born with low copper, and bloodwork revealed it was dropping at an alarming rate. Andrew asked me if I had any suggestions of what might help this child,” explains Sarkar.
Based on all of Sarkar’s work and his discovery that copper-histidine was biologically available in human blood, he proposed that the baby receive an injection of copper-histidine. His years of attending clinical rounds suddenly demonstrated their worth. He knew that since children with Menkes disease cannot absorb copper, copper-histidine could not be given orally and would need to bypass the gut and be administered via injection.
Knowing this was a fatal disease with no treatment options, Sass-Korstak presented this novel treatment option before SickKids’ Committee of Clinical Investigation, which would have to be the Research Ethics Board of that time, and it was approved as an experimental drug. With consent from the family, the medical team led by Sass-Korstak proceeded with this treatment plan, as it was the only option for this sick baby. This was the world’s first Menkes patient to receive copper-histidine therapy in 1976.
“Slowly the baby’s copper levels increased. His health improved and by three years old he was climbing stairs and growing normally, while previously children with Menkes would have died by this age,” says Sarkar.
After this first case, SickKids saw its second successful case in 1986 and delivered the same early treatment of copper-histidine with the same positive patient outcome. By this time, Sarkar had been working with SickKids pharmacist Karen Walsh to develop a standard formulation and clinical protocol so other centres could learn how to prepare the copper-histidine and help kids outside of SickKids.
Copper-histidine is not a cure for kids with Menkes disease, but if administered very early, before neurodegeneration has begun, it can have a huge impact on the child’s growth, brain development and life expectancy. However if the children are not diagnosed as babies, copper-histidine cannot reverse the brain damage that has already been done.
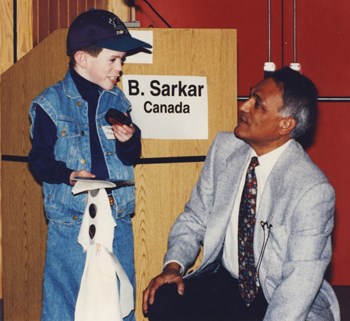
Sarkar continued to research and publish on Menkes disease and spoke all around the world including giving an invited lecture in Nobel Symposium in Sweden in 1982 on Inorganic Biochemistry, a newly emerging discipline in science. Thanks to the early spirit of collaboration between Sarkar and Sass-Korstak, the life expectancy for kids with Menkes disease went from just three years old to early adulthood. The oldest documented case (2012) describes a 34-year-old man.
“Coming to SickKids offered me the opportunity to apply my basic science expertise to medical problems. I could have kept my head down in my lab and focused on my own work. But I was encouraged to pursue questions and learn about things outside of my field. This led to discovery and ultimately changed how Menkes patients are cared for to this day,” says Sarkar. “This spirit of collaboration lives on, I’ve seen it over my 53 years here and continue to foster it among young clinicians and scientists, alike. I have approached teaching similar to how Andrew mentored me, and encourage young scientists to appreciate and use the connection to the hospital as a motivator and driver for their work."
And his successors have paid heed to the importance of collaboration, just four years ago, SickKids research was conducted in labs and offices scattered across Toronto’s Discovery District. The promise of new, state-of-the-art research tower was to bring all of SickKids’ scientists into one building to build on this rich culture of collaborative science that has existed since the founding of the Research Institute. The Peter Gilgan Centre for Research and Learning opened its doors in September 2014 and is the home to more than 2,000 SickKids scientists, trainees and research staff.
Key publications
- 1966: “Copper-amino acid complexes in human serum” published in Biochemistry of Copper, New York. Academic Press, 1966; 183-196.
- 1993: “Copper-histidine therapy for Menkes disease” was published in the Journal of Pediatrics 123, 828-830 (1993) detailing the formulation of copper-histidine for injection
- 1996: “Early copper-histidine treatment for Menkes disease” published in Nature Genetics, 12, 11-13 (1996) Sarkar and research team in Denmark did gene analysis of Menkes patients. Their results showed that the SickKids patient cases had severe mutations that resulted in a truncated copper transport protein. If copper histidine was not given, they would have died. This was the final proof.
- 1998: “Early treatment of Menkes disease with parenteral copper-histidine: long-term follow-up of four treated patients” published in the American Journal of Medical Genetics. 76,154-164 (1998) detailing a long term clinical follow up of four early copper-histidine treated patients from Canada (SickKids), Switzerland and Australia aged 20, 18, 10.25 and 10 years respectively. Neurologically the patients all did well but in some cases connective tissue and skeletal abnormalities could not be corrected. Early diagnosis and treatment as well as the type of disease mutation seem to determine the outcome of treatment.
- 2004: “X-ray Structure of Physiological Copper(II)−Bis(L-histidinato) Complex” published in Inorganic Chemistry 43, 3338-3340 (2004) shows its unique structure.


