Spina bifida repaired in-utero
Summary:
In a Canadian first, a team from Mount Sinai Hospital and SickKids has repaired a form of spina bifida in a fetus at 25 weeks gestation.
First in-utero surgery in Canada for the treatment of spina bifida a success
TORONTO – In a Canadian first, a team from Mount Sinai Hospital and The Hospital for Sick Children (SickKids) has repaired a form of spina bifida in a fetus at 25 weeks gestation. The baby’s mother, Romeila Son, recovered very well from surgery, and a bouncing baby girl, Eiko, weighing 2.45 kg, was born on August 19 at 36 weeks gestation at Mount Sinai Hospital. Since her birth, Eiko has needed no further intervention for this usually debilitating condition. This is the first case in Canada where the mother has not had to travel to the United States for this specialized surgery.
Dr. Greg Ryan heads Canada’s largest and most experienced fetal therapy program at Mount Sinai Hospital and Dr. James Drake heads Canada’s largest and most established neurosurgical centre for the postnatal repair of spina bifida at SickKids. Working in collaboration with colleagues from Vanderbilt University in Nashville who pioneered the procedure, a team of 24 clinicians led by Drs. Ryan and Drake successfully carried out the 2.5 hour in-utero procedure at Mount Sinai on June 4, 2017.
Myelomeningocele is a form of spina bifida, affecting approximately 120-150 babies in Canada each year. It is caused when the spinal column fails to close early in fetal development, causing permanent damage to the baby’s spinal cord and nervous system.
Babies with spina bifida can have varying degrees of paralysis of their lower limbs and many will need mobility supports such as leg braces, crutches or wheelchairs. Over 80 per cent of children with spina bifida will require a shunt to be inserted to relieve pressure on their brain, which must remain in place for their entire life, and some affected children will have a negative neurocognitive outcome. Between 15-30 per cent of children with spina bifida do not survive into adulthood and less than 50 per cent live independently as adults. A third of adults with spina bifida require substantial lifelong daily support. The emotional, social and financial impact for these affected individuals, their families and society as a whole, is enormous.
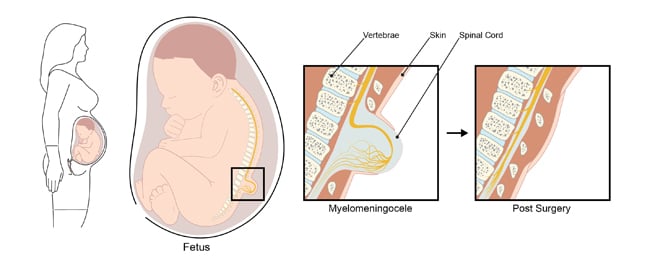
The Management of Myelomeningocele Study (MOMS), a groundbreaking trial published by Vanderbilt University, Children’s Hospital of Philadelphia and the University of California, San Francisco, in the New England Journal of Medicine in 2011, showed that, in babies who underwent the in-utero procedure:
- Brain malformations were reversed by one-third
- The need for walking aids or a wheelchair was halved
- Their need for brain shunts was reduced by half
Consequently, the Society of Obstetrics and Gynaecologists of Canada (SOGC) now mandates that any pregnant woman whose fetus has spina bifida must be counselled about this treatment option.
How it was done
The mother, Romeila, was put under general anaesthesia.On June 4, a joint clinical team of surgeons, anaesthesiologists, neonatologists, fetal medicine specialists, cardiologists and nurses assembled in the High Risk Obstetrical Operating Room at Mount Sinai Hospital, part of the Frances Bloomberg Centre for Women’s and Infants’ Health.
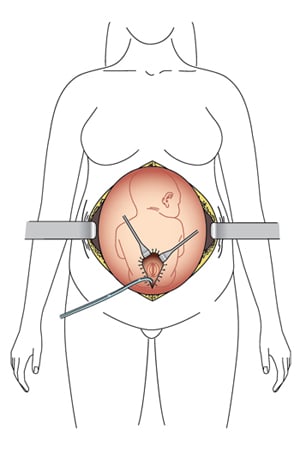
- The fetus was temporarily sedated, anaesthetized and paralyzed via a fine needle through her mother’s abdomen.
- Abdominal and uterine incisions were made by Drs. Ryan and Tim Van Mieghem from Mount Sinai’s fetal medicine team under ultrasound guidance, avoiding the placenta.
- The fetus was carefully maneuvered into position to expose her back, with the team constantly monitoring amniotic fluid levels and vitals of mother and baby. A fetal cardiologist continuously monitored the baby’s heart function.
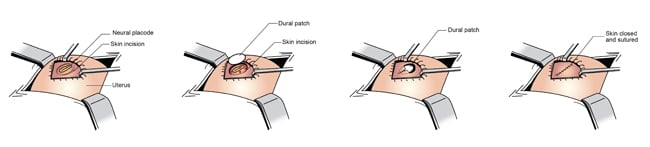
- Drs. Drake and Abhaya Kulkarni from SickKids began the neurosurgical component of the procedure by dissecting out the neural placode from the surrounding tissue. An artificial dural patch was then placed over the exposed neural tissue. The surrounding skin was freed up, allowing it to be closed over the spinal defect. The neurosurgical portion took 25 minutes.
- Drs. Ryan and Van Mieghem closed the uterus, taking great care to create a watertight seal to ensure that there was no leakage of amniotic fluid.
- Romeila was admitted to Mount Sinai’s high risk inpatient antenatal unit for two weeks.
- The birth of baby Eiko occurred by Caesarean section at Mount Sinai on August 19.
Mount Sinai Hospital and SickKids recently collaborated on another in-utero surgical first, repairing a congenital heart defect called transposition of the great arteries, in May, 2017. The team from SickKids and Mount Sinai Hospital is Canada’s only provider of fetal surgery.
Quotes
“I am extremely proud of the collaboration between Mount Sinai Hospital and SickKids – which has resulted in a terrific outcome for this baby girl. Although fetal surgery will not be appropriate for all fetuses with spina bifida, it is extremely encouraging that, for some, it may preserve neuromotor function, reverse brain herniation and reduce their need for a brain shunt. However, it also entails some maternal and fetal risks, particularly that of premature labour, which must be carefully balanced. Having this kind of clinical capacity here in Ontario will really change the range of options available to parents who have been given a diagnosis of spina bifida during pregnancy,” says Dr. Greg Ryan, head of the fetal medicine program at Mount Sinai Hospital, part of the Frances Bloomberg Centre for Women’s and Infants’ Health.
“We regularly see children who have been affected by spina bifida at SickKids. It is my hope that our capacity to perform this in-utero surgery here in Toronto will mean that we can optimize their clinical outcomes, and reduce the degree of medical challenges these children will face,” says Dr. James Drake, head of the division of neurosurgery and senior associate scientist at SickKids.
“I would like to congratulate everyone at Mount Sinai Hospital and SickKids who teamed up to perform Canada’s first in-utero spina bifida surgery. The incredible story of baby Eiko’s journey into this world shines a bright light on our world-class health care professionals. They're talented, innovative, and making life better for people in this province — starting even before they’re born. Congratulations to little Eiko and her family. I wish them a healthy, happy future.” Honourable Kathleen Wynne, Premier of Ontario.
“In my practice at Holland Bloorview Kids Rehabilitation Hospital, I work with children who, through their determination and perseverance, seek a better quality of life with spina bifida. As an adult with spina bifida myself, I am both professionally and personally excited about the potential of this procedure and the impact it can have,” says Dr. Paige Church, who leads the spina bifida clinic at Holland Bloorview Kids Rehabilitation Hospital. The clinic, which provides rehabilitation therapy for kids with spina bifida, is one of the largest of its kind in Canada with over 250 children seen annually and growing.

