How SickKids’ new MAGIC clinic is transforming urinary and colorectal care
Summary:
A multidisciplinary clinic for children and adolescents with congenital and acquired conditions of the pelvis is bringing “life-changing” care closer to home.
Elaine* had already arranged one trip to an American hospital for specialized care for her son Ryan* when she asked a doctor at The Hospital for Sick Children (SickKids) to help fill out the OHIP paperwork to cover a second trip.
Ryan was born with a birth defect called anorectal malformation, in which the lower end of his digestive tract didn't develop properly. Like most children who have anorectal malformations, he experienced chronic constipation. In an effort to allow him to have regular bowel movements, he had surgery as a newborn – but because of complications from that surgery, he had little control over his bowels and had daily accidents.
As Ryan was approaching school age, Elaine and Ryan visited the American hospital’s week-long bowel management program on the recommendation of Ryan's doctor at SickKids. There, doctors determined the best solution for Ryan was a daily enema – a liquid placed into the rectum to flush out the stool that has built up in the bowel. It was awful for Ryan, Elaine recalls. She asked herself: “How am I going to do this for the rest of his life?”
The American doctors had offered a more long-term solution: an appendicostomy, or Malone antegrade colonic enema (MACE), a surgery where a passage is made between the abdomen and the colon, using the appendix. This allows the enema to be given at the beginning of the colon, instead of the rectum. It would be life-changing for Ryan, Elaine realized.

During Ryan’s next appointment at SickKids, Elaine planned to ask for support with the OHIP application to get the MACE surgery in the U.S. The doctor who previously helped her was retiring, so this time she met with Dr. Rodrigo Romao, a surgeon in the divisions of general surgery and urology who’d come to SickKids to strengthen the hospital’s pelvic colorectal specialty.
“OHIP will not cover this surgery being done in the U.S.,” Elaine remembers Romao telling her.
“Why?” she asked, and he said, “Because we can do it at SickKids.”
Elaine was “elated.” The surgery was booked as soon as possible, in March 2024. As she hoped, the surgery was “life changing.” Now Ryan, who is six, can “have a sense of dignity and independence” as he does his daily “flush” by himself.
“It was sort of like magic”
Ryan’s follow-up care is provided through a brand-new clinic Romao started this year at SickKids: the MAGIC clinic, which stands for Multidisciplinary Anorectal Genitourinary Improvement of Continence. Romao and the team picked the name thoughtfully – they wanted it to be something uplifting that didn’t downplay patients’ experiences with complex congenital and acquired conditions of the pelvis like anorectal malformation, Hirschsprung’s disease and bladder exstrophy.
The clinic’s name has resonated with staff and families alike. It makes Ryan feel less anxious to hear he’s going to the MAGIC clinic, Elaine says – and it represents the impact of his care at SickKids: “It was sort of like magic.”

From left to right: Abby Varghese, Noreen Goraya, Dr. Rodrigo Romao, Dr. Pippi Salle, Dr. Jacob Langer, Monping (Ping) Chiang, Sherri Jarvis, Dr. Michelle Gould and Dr. Michael Chua.
Before the creation of the MAGIC clinic, care for these patients was often fragmented, Romao says. That’s why the clinic brings together staff in general surgery, urology, gastroenterology, gynecology, social work and nursing. This allows patients to see several clinicians together in one visit, saving them multiple trips to the hospital. It also ensures patients’ care is tailored to their needs, a cornerstone of SickKids’ Precision Child Health movement. The team is all together in the room for clinical consults, and they share their thoughts on next steps there so the patient and family can listen and participate. That makes the care “more individualized and catered to patients,” says Abby Varghese, one of the clinic’s nurse practitioners.
Since starting in March 2024, more than 230 patients have visited the MAGIC clinic. This includes referrals from other Ontario hospitals and more than a dozen out-of-province referrals. The clinic benefits from the support and experience of Dr. Pippi Salle, a paediatric urologist who provides mentorship and coaching in complex pelvic reconstructive cases and Dr. Jacob Langer, a paediatric general surgeon who is retired but still attends some MAGIC clinics and assists with difficult colorectal cases. Dr. Michelle Gould, a paediatric gastroenterologist, is also an essential part of the team, bringing her expertise in motility disorders, conditions affecting the gastrointestinal tract.
While the MAGIC clinic doesn’t “magically fix” what patients and families are struggling with, it does provide comprehensive care, notes Monping (Ping) Chiang, another nurse practitioner with the clinic.
“It gives resources and support,” she says. “That’s what, to me, the MAGIC clinic can do – help families through certain stages, depending on the child’s development, and know there’s a team who knows their child, and their complex diagnosis, really well.”
A holistic approach
Romao knows the patients he sees in the MAGIC clinic can struggle later in life. He emphasizes a holistic approach to care, including a focus on the emotional well-being of patients and their families.
The MAGIC clinic team includes a social worker, Noreen Goraya. She notes some of the children and youth who come to the clinic might have had decisions impacting their bodies, like having a certain surgery or procedure, made for them when they were young. In talking to patients about the impact of their care on their everyday lives, like with friends or at school, she can learn a “golden nugget” that she can share with the team to inform their care.
“Some information might not come out when talking to the medical team,” she says. “So it’s important to give that sense of control and agency, to know that something isn’t going to happen without their voice.”
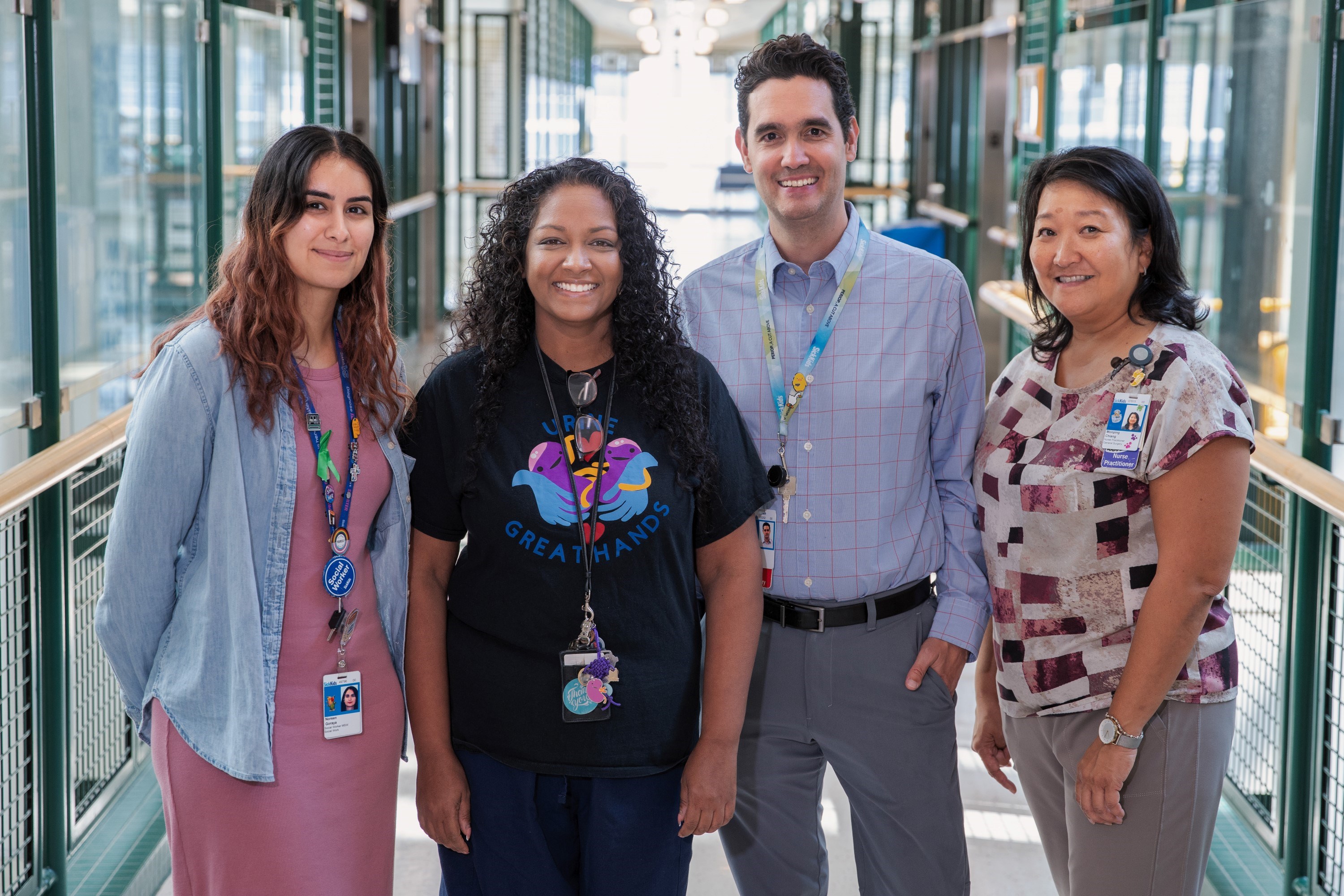
From left to right: Noreen Goraya, Abby Varghese, Dr. Rodrigo Romao and Monping (Ping) Chiang.
For the mom of one MAGIC patient, the team’s personable approach stands out. Meghan’s son Robert was born last year and has Hirschsprung’s Disease, a condition where nerve cells are missing from part of the bowel. He had a “pull through” surgery in February to remove the part of the bowel that was missing nerve cells but needed an emergency stoma and colostomy soon after. The stoma gave his bowel time to rest from the original surgery, and he had a third surgery in June to reverse it. Meghan says Romao and the team helped her feel confident and empowered in managing Robert’s care at home.
“The MAGIC clinic has done a really good job at making this journey less overwhelming for me,” she says.
At follow-up visits at the clinic, she’s appreciated the way the staff further support her and Robert.
“You feel like they care about you, like you’re part of their family. They don’t make you feel forgotten,” she says. “Knowing that support’s there, and that they are always reaching out their hand to see if we need anything, is absolutely amazing.”
Embracing patient voices
Before the MAGIC clinic, teenage SickKids patient Isabella* spent time during her summer school breaks travelling to the U.S. to receive care at a hospital there.
“I didn’t really know any of the doctors there, so it was pretty uncomfortable,” she says.
Now, she’s excited to be able to access the comprehensive care she needs at SickKids. Not only does it save her and her mom Amy* a trip to the U.S., but it brings together the multiple clinics she used to see separately at SickKids.
“It makes sense to have all the clinics together, because in the part of the body they’re focused on, everything affects everything else,” she says. “When all the clinical team members are in the same place, they all have the knowledge of what’s going to interact with what.”
“We want everyone with expertise putting their heads together to think about what’s best for these kids,” Amy says. “They’ve created the infrastructure by coordinating the schedules, allowing different specialties to weigh in and discuss Isabella’s specific case. This is exactly what we want.”
While Romao hopes to model the SickKids clinic after the U.S. hospital Centres of Excellence, like the ones Isabella previously visited, Amy says other hospitals can learn from the way SickKids embraces listening to the voices of patients and families and building relationships with them – another key piece of Precision Child Health.
“I think SickKids is going to take this specialty much further, because they’ve already embraced that shared decision making,” she says.
Goraya, the clinic’s social worker, says the team really wants patients to feel their voices are heard, because they are the experts in what they are going through.
“Being in that room can feel daunting, so it’s very empowering to step into their experience and feel confident.”
You might even say it’s magical.
*Names have been changed for patient privacy

