SickKids team discovers overconnected brain cells may cause autism
Summary:
Typically nerve cells with fewer connections are associated with autism. A team at SickKids found that nerve cells from children with autism can be overconnected and overactive, leading us to think about the causes of autism in a new way.
New study uses stem cells to show nerve cell overconnectivity and overactivity in autism
Autism is associated with alterations in many genes. When a gene is altered, it can affect how the nerve cells in the brain work. The human brain contains billions of nerve cells that communicate with each other through specialized points of contact known as synapses. On average, each nerve cell is connected to 1,000 other nerve cells, creating nerve cell networks that serve different brain functions. Too much or too little connectivity between nerve cells can lead to various neurodevelopmental disorders. Until recently it has not been possible to directly test the impact of a genetic change on the shape and function of human nerve cells.
A research team at The Hospital for Sick Children (SickKids) led by Dr. James Ellis, Senior Scientist in Developmental and Stem Cell Biology, and Dr. Michael Salter, Chief of Research and Senior Scientist in Neurosciences and Mental Health, tested how alterations in a gene called SHANK2 affect human nerve cells derived from individuals with autism.
“These results are significant because we found that nerve cells from children with autism can be overconnected and overactive when SHANK2 is altered,” says Ellis, who is also Professor, Department of Molecular Genetics at the University of Toronto. “It shows the power of using stem cells to produce and study human nerve cells that cannot be obtained in other ways.”
The team reprogrammed skin or blood cells from two families with autism to produce stem cells that were matured in the lab to make nerve cells. Then they compared the autism nerve cells to unaffected controls, and together with Dr. Stephen Scherer, Director, The Centre for Applied Genomics and Senior Scientist at SickKids, the results were confirmed using gene editing to correct or create changes in SHANK2.
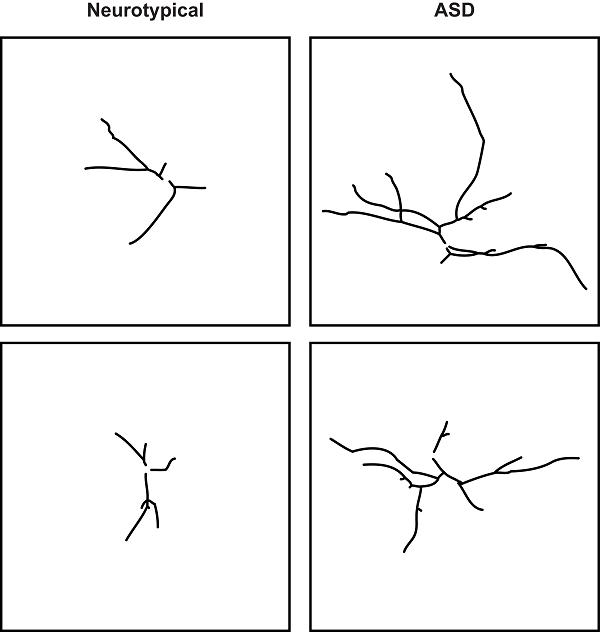
“If the brain cells are like trees, we typically see fewer branches and leaves in children with autism,” says Scherer, who is also Professor, Department of Molecular Genetics at the University of Toronto. “Our findings show the exact opposite – an abundance of branches and leaves – leading us to think about the causes of autism in a new way.”
The key findings by co-first authors Kirill Zaslavsky, MD/PhD Student at SickKids and the Department of Molecular Genetics at the University of Toronto and Wen-Bo Zhang, Research Associate at SickKids are reported in Nature Neuroscience. Zaslavsky found that the human SHANK2 nerve cells are longer and have more complex dendrites that reach out from the cell body to connect with other nerve cells, and these dendrites have more connections called synapses to transmit chemical signals which are translated into electrical signals in targeted nerve cells. Zhang found that this evidence for overconnectivity was accompanied by more electrical activity in SHANK2 nerve cells compared to the unaffected controls.
The families were excited to hear an update on the findings from the research study. “More than anything, when we decided to be part of this study back in 2010, we wanted to help our son Jack. But if that’s not possible, we wanted to be part of something greater that can help other families in the future,” says Amy Perkins, whose family’s cells were donated for this research.
The altered gene regulation and compound testing provide insight into the how the nerve cells become overconnected, and this may help guide research into how to prevent these changes from occurring. In related stem cell research published in the open-access journal, eLife in February, Scherer and Ellis demonstrate that alterations in two other autism genes also lead to increased electrical activity in nerve cells.
The strength of the stem cell based approach is that it produces human nerve cells to study autism in the lab. However, these nerve cells are at an early stage of development and are not yet equivalent to nerve cells in children or adults. The changes seen in the lab may have occurred prior to the behavioural changes related to autism, and this may limit the translation of the research into clinical settings.
This research was funded by the Ontario Brain Institute, the Canadian Institutes of Health Research, the National Institutes of Health, Simons Foundation Autism Research Initiative (SFARI) and SickKids Foundation. This study is an example of how SickKids is making Ontario healthier, wealthier and smarter (www.healthierwealthiersmarter.com).

